To many people, yellow fever is a disease from a bygone era in which giants like Benjamin Rush and Walter Reed roamed. Indeed, since yellow fever was beaten back from the United States and many other areas of the world and an effective vaccine was developed (and resulted in a Nobel Prize) yellow fever is largely thought of as a travel-related disease. However, new and recent outbreaks of the disease in various countries -- including its first ever Asian appearance in China -- and poor vaccine supply chains and logistics have increased the threat level posed by this virus. As the virus is spread by the Aedes aegypti mosquito (aka the yellow fever mosquito) to which half the human population is exposed to yellow fever has the capacity to roar back. With a penchant for severe disease and death, such an event would be majorly disruptive.
Yellow fever outbreaks are managed by effective vector control and vaccination campaigns. However as the frequency of these outbreaks occurs and the population sizes involved increase, it is increasingly likely that vaccine supply issues will constrain the ability to respond. Coupled to that supply issue -- which is even impacting the US -- is the logistical issues that constrain vaccine administration.
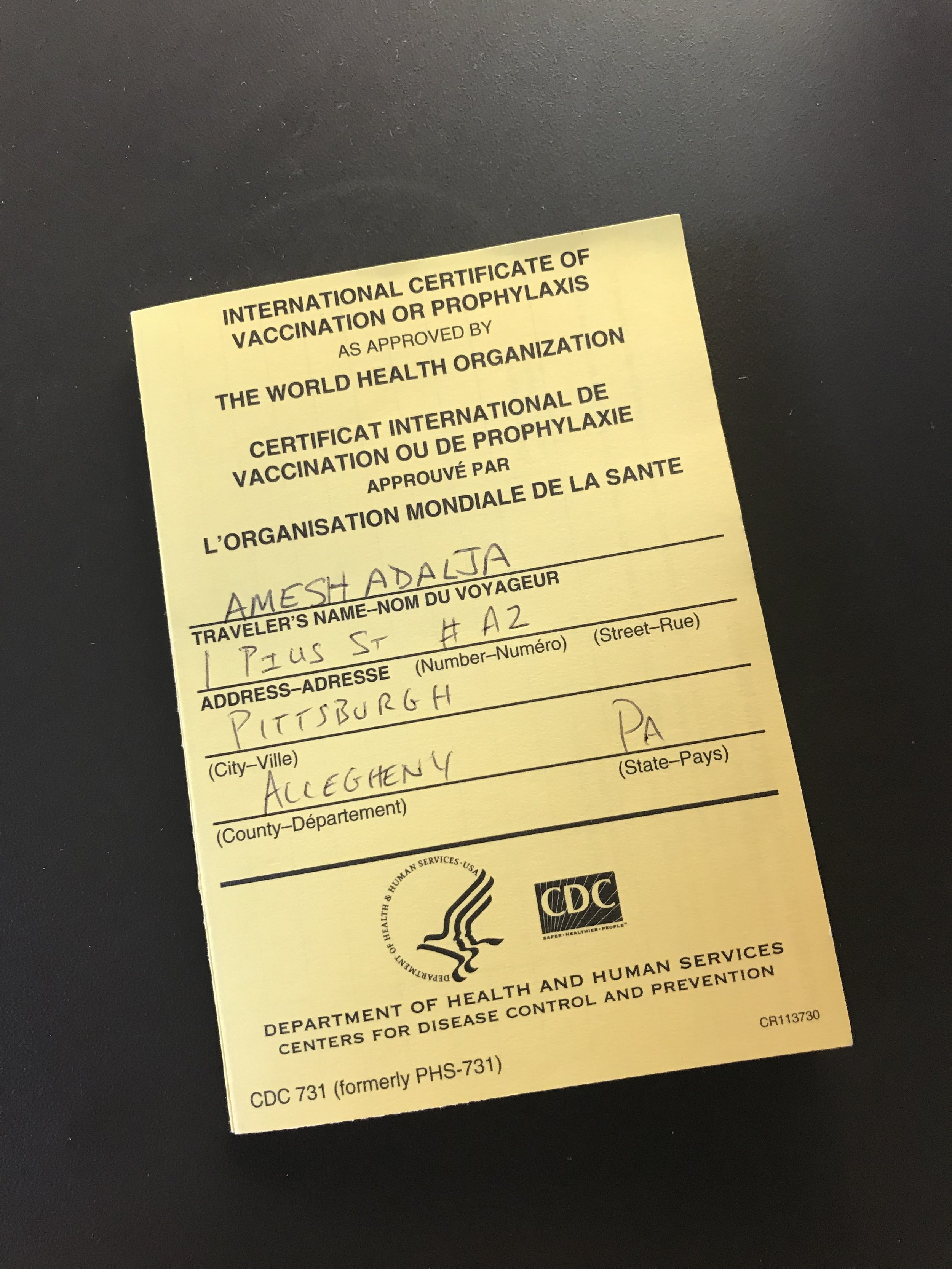
Yellow fever was one of the original infectious disease covered by the International Health Regulations (IHR) given its high consequence nature. As part of the IHR framework, yellow fever vaccines have to be administered by certified vaccine centers in every country, including the United States. In the US, certification is done on a state level.
While all this may just seem like a minor hurdle to overcome, my experience last week procuring vaccine for myself and a couple of others left me wondering if this regulatory framework could hamper response efforts in an emergency situation that is already compromised by vaccine supply issues. Suffice it to say arranging a vaccination for a pediatric patient in Pennsylvania -- even when you are an infectious disease physician -- was daunting and really frustrating. The amount of paperwork the vaccinator has to fill out and the consequent amount of time one must wait for vaccination was almost prohibitive to someone as pathologically impatient as me.
In emergency infectious disease situations, bureaucratic inertia can rapidly make a tenuous situation worse and delays only benefit pathogen spread. If a yellow fever outbreak took hold in the US vaccination would be increasingly demanded and, just like during a flu pandemic, easily accessible vaccination points employing physicians, nurses, pharmacists, and other health care workers would be ideal in order to maximize vaccination coverage.
Relying exclusively on certified yellow fever vaccinators, to comply with IHR stipulations, could prove difficult in such a situation. In addition, state laws -- such as exist in Pennsylvania -- artificially restricting the age limits a pharmacist can vaccinate (because 17 year olds are somehow magically different than 18 year olds) will also pose problems as it does in every outbreak situation in which pharmacist-administered pediatric vaccination stipulations have to be waived.
I understand the real problem posed by fake yellow fever vaccinators and the black market in counterfeit yellow fever vaccination certificates, but a one-size-fits-all approach that could hamper the US ability to fortify itself against yellow fever is not optimal.